How to describe neurofatigue. Unless you have a brain injury, it’s almost impossible to explain.
Neurofatigue is one of the biggest and long-lasting effects of a stroke. When I was in the hospital, no one said the word neurofatigue to me. My husband, Tommy, never heard it either. The nurses would explain that extended periods of rest are expected following a stroke but never that it would be long-lasting.
The day I was released from the hospital, we stopped at Walmart. We were only there for fifteen minutes, but the exhaustion that followed was indescribable. The fatigue that followed my stroke was debilitating, forcing me to nap after even the simplest tasks, like showering or vacuuming a single room.
Soon after my stroke, a person said to me that if I didn’t stop napping, I would become dependent on them. I knew from what the nurses told me that this was normal, so I started googling. This is where I learned about neurofatigue.
My speech therapist connected me with another young stroke survivor on Cape Breton Island, and she gave me the following links:
I sent these to anyone who I felt needed to know.
Unfortunately, resting is part of recovery. Almost 2 years after my stroke, if I don’t have one nap per day, I can’t fall asleep that night. My brain is way too over-stimulated to rest, leading to a weird feeling of anxiety.
So far, neurofatigue has limited how far I can drive. After 45 minutes, I have to turn the wheel over to another driver, and my brain is depleted for the day. I can’t talk properly, lose words, find it hard to complete a sentence. This is frustrating. Living in a rural area, when my partner is working out of town, I must find individuals to drive us to appointments such as the dentist and orthodontist, which are more than an hour away. When my daughter plays sports out of town, I cannot take turns driving. I can no longer jump in the car and head to Sydney or Halifax for shopping, to pick someone up at the airport, or to visit friends and relatives.
Meeting in a group does NOT drain my brain. Meeting one on one does. A friend was visiting town recently, and we hung out by ourselves on two occasions. I thoroughly enjoyed our time together, but my neurofatigue hit me much sooner on those days. (Sorry friend…it’s not you…it’s me! 😉)
Recently, my teenage daughter has been wanting to talk in the evening. Wanting to talk to ME! Isn’t this every mother’s dream? At that time of day, I am mentally exhausted and can barely articulate a coherent thought. The other night I told her to come find me earlier in the day, so we can actually have a proper conversation.
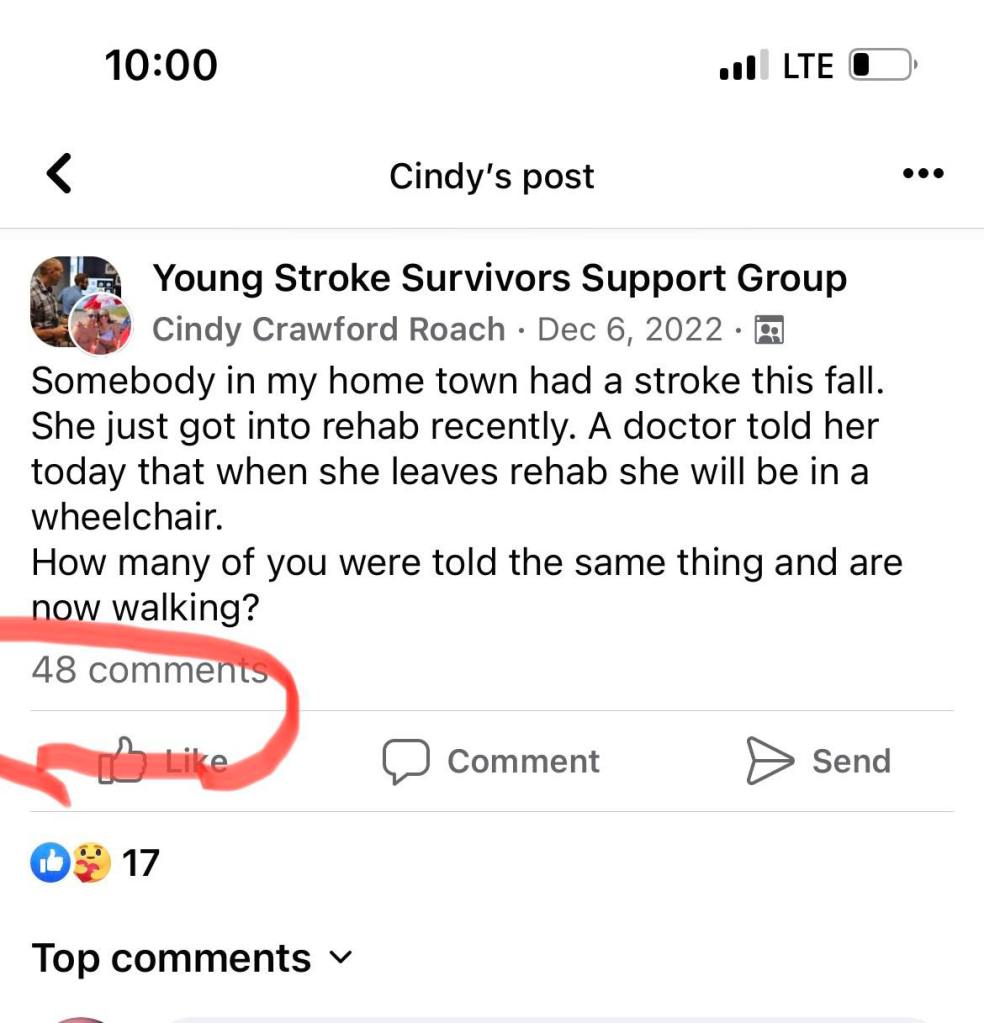
When I decided to write this blog topic, I tried to find the perfect quote that illustrates neurofatigue. From the standpoint of a stroke survivor, I couldn’t find one that truly fit. I put this post on the Young Stroke Survivors Facebook group:
I am writing a blog post about neurofatigue. The explanations I find describing neurofatigue just don’t cut it. How would YOU describe it?
There were 40 responses. Here are some of them.
Tiffany Brunner: It is like hitting a literal wall. The closer you get to it, the more you notice all your effects from the stroke. You can’t focus, you can’t think. You start making mistakes. Forgetting words, stumbling thoughts. Once you finally hit that wall. It’s a kind of tired that your eyes start to water, and there’s nothing you can do except go to sleep. Feelings of shame and guilt…depression because you can’t do what you used to do.
Reesa Fletcher: My husband says it’s like watching a cell phone battery. The battery being me. I start out strong, alert and responsive. As the day progresses, the response is slower, thinking is slower, production grinds to a halt. Inside, I feel myself in a fog. My thinking and responding is delayed. Tired, the need to shut down and sleep. It’s like being drugged. It will hit me hardest when I problem solve my day, drive, concentrate for long periods. Simple tasks that I could do before are a major daily task.
Ashley Sandler: For me, it’s a constant longing to sleep, no matter how much I’ve already slept. It’s being a lifelong mathematician and not being able to calculate simple equations. It’s being a book lover and not be able to make it through one page remembering any of the words I’ve just read. It’s reminding myself that it’s okay to just breathe when everything else just takes too much energy. The person I AM =/= The person neurofatigue allows me to be.
Nicky Hopkins: There is no rhyme or reason to it and I can’t predict it. It just hits and it feels like whole body exhaustion – like flu without the cold. I know it’s coming when suddenly my words get muddled. The only thing that solves it is rest and sleep.
Ryan Malynn Becker: Exhaustion deep in your soul. To your core. Not sleepy, just can’t take another step tired. The battery being so drained it cannot recharge. I’ve said it before but us warriors need our own dictionary. Because tired doesn’t mean the same anymore!
I have been so fortunate with my support system. Everybody around me understands neurofatigue and my limits. My husband continues to be amazing.
Not every stroke survivor is so lucky! I see countless posts on the Stroke Facebook page of survivors who receive no compassion or understanding of neurofatigue or their recovery. Some stroke survivors are compared to other survivors by their support system.
“This person was fine after so much time…what’s wrong with you?”
“I know you had a stroke but you are home now, so get over it!”
Every stroke survivor has different deficits and different rates of recovery. Some recover fully. Most do not. Recovery takes so long. Families! Please be patient and supportive. Your stroke warriors will be grateful.
I wish I had been given a book when I left the hospital, explaining neurofatigue, auditory overload, common sensory problems at social functions, and other deficits to be aware of, along with practical suggestions or helpful tips. Maybe I will write one!